Predicting the Development of Alzheimer’s Disease with Artificial Intelligence

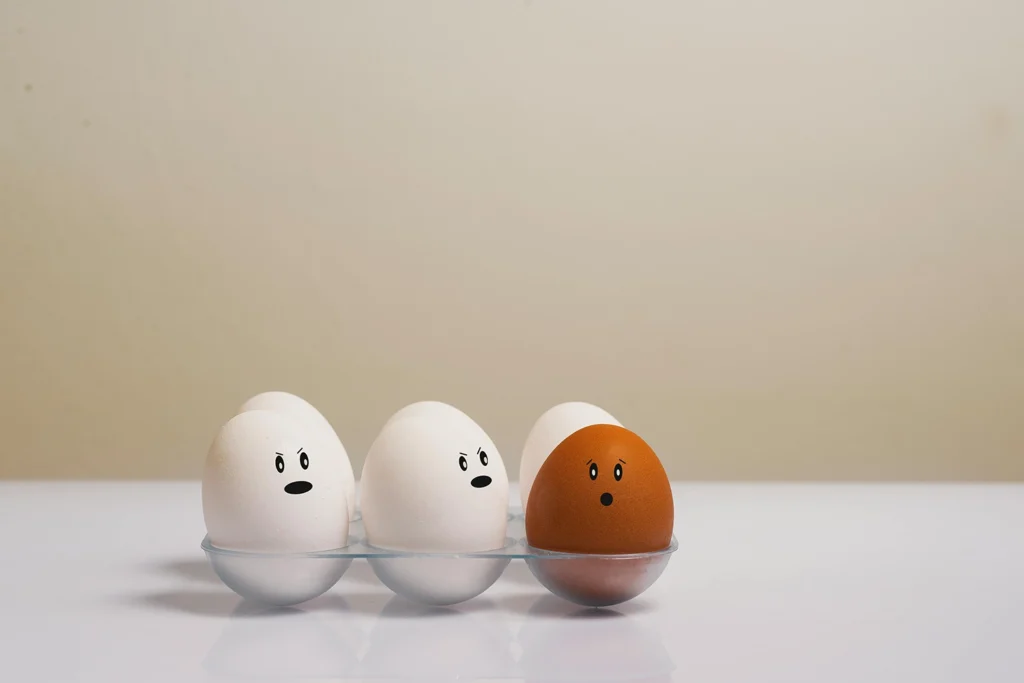
How Discrimination Gets Under the Skin
This Common Nutrient Deficiency Is More Prevalent in Women

Why is ADHD Becoming More Common in Adults?
A Revolutionary Way to Estimate Biological Age and Predict Health Outcomes

The Fiber Effect: A New Era in Gut Wellness

The Importance of Strength Training for Women

The Emerging Science Replacing the “Leaky Gut” Idea

Neural Synchronization
