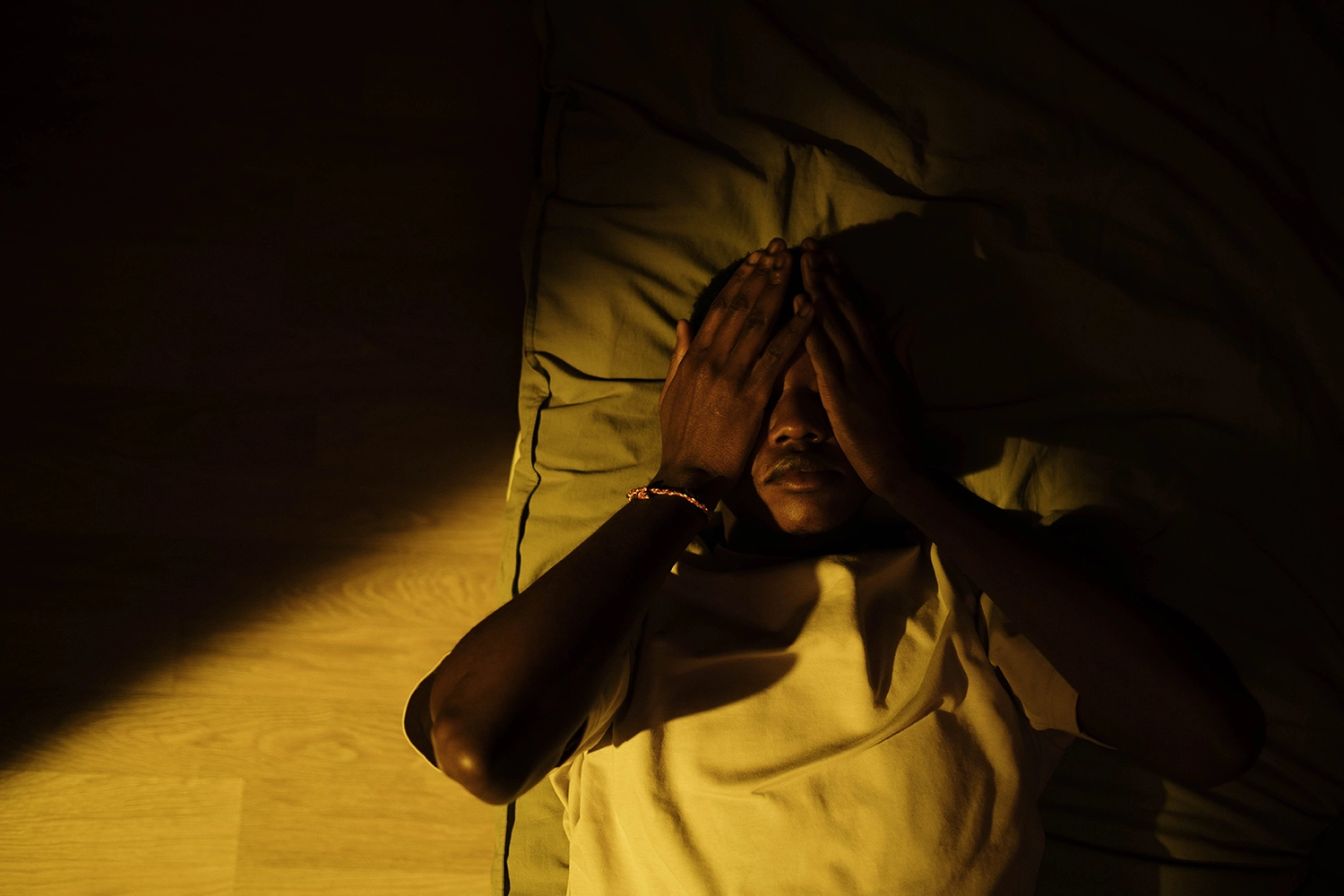
How Can Cognitive Behavioral Therapy (CBT) Help with Insomnia?
PREMIUM CONTENT for MEMBERS ONLY
Almost 1 in 5 American adults regularly use sleeping pills to manage sleep disorders like insomnia, which affects about 10% of the population. Insomnia makes it difficult to fall asleep or stay asleep, and often leads to waking up too early, and not being able to fall asleep again and awakening in the morning not feeling rested.
Insomnia and poor sleep are not only unpleasant and annoying, but a compromised sleep rhythm can have serious health consequences, increasing the likelihood for metabolic diseases including type 2 diabetes, but also increasing the risk for common chronic diseases, like metabolic syndrome, obesity, cardiovascular diseases and early cognitive decline. As the interactions of the gut microbiota with the gut are synchronized with the sleep diurnal rhythm, interrupted sleep pattern can also affect the communication between the microbiome and the gut.
While some sleeping pills can provide short-term treatment by increasing GABA, an inhibitory neurotransmitter in the brain, they are typically not as effective for long-term treatment for insomnia. On the other hand, Cognitive Behavioral Therapy (CBT) is a well-researched treatment for long-term sleep problems like chronic insomnia. Unlike sleeping pills, CBT addresses the root cause of sleep disorders by identifying thoughts and behaviors that contribute to sleep problems. Cognitive behavior for insomnia focuses on several core strategies, some of them including sleep restriction therapy, stimulus control therapy, and sleep hygiene.
“Sleep Restriction Therapy aims to address this problem by limiting sleep opportunity to the patient’s average sleep ability,”
Chronic insomnia can be perpetuated by sleep extension, which is the tendency to stay in bed longer to compensate for lost sleep. This creates issues between sleep ability, which is the number of hours you actually sleep, and sleep opportunity, which is the number of hours you have available to sleep. The Sleep Restriction Therapy aims to address this problem by limiting sleep opportunity to the patient’s average sleep ability. As a result, the drive to sleep increases and the time to fall asleep decreases. Sleep Restriction Therapy can be completed in four steps:
- Determine your baseline sleep ability through daily sleep diaries over two weeks
- Set the prescribed time in bed equal to the average sleep duration
- Determine a morning rise time that you can adhere to
- Set the prescribed time to bed by subtracting the prescribed time in bed from the desired wake-up time.
This gathers enough data to calculate a sleep efficiency percentage that can determine how much time you should spend in bed to improve sleep time. The first week of this therapy sound difficult and may feel tiring, as it may involve only being in bed for six hours. However, after about a week most people can decrease their time spent awake in bed and improve their sleep quality.
“…behaviors [like reading in bed or watching television] can reinforce the association between the bedroom and wakefulness.”
Unlike sleep restriction therapy, Stimulus Control Therapy (SCT) is based on cognitive behavioral principles. It operates on the idea that a single stimulus can lead to various responses, depending on their associations. In healthy individuals, stimuli related to sleep, such as the bed or the bedroom, are associated with sleep. However, in patients with insomnia, these same sleep-related stimuli become associated with other activities like reading, watching television, and staying awake in bed while attempting to sleep. This leads to a maladaptive conditioning pattern that reduces the likelihood of sleep happening when and where the patient wants (at night and in the bedroom). In fact, these behaviors can reinforce the association between the bedroom and wakefulness. To address this, SCT recommends (1) lying down only when feeling sleepy, (2) avoiding using bed time for activities other than sleep, (3) getting out of bed if unable to sleep within 15-20 minutes and returning only when sleepy, (4) repeating this as necessary throughout the night, (5) waking up at the same time every day, and (6) avoiding napping during the day. These recommendations form the foundation for developing good sleeping habits and should be followed even after better sleep is achieved.
“[Practicing sleep hygiene] can positively impact their sleep quality by providing information about behaviors that affect sleep.”
Another important component to CBT treatment for insomnia is sleep hygiene. Educating patients on proper sleep hygiene practices can positively impact their sleep quality by providing information about behaviors that affect sleep. Generally, sleep hygiene outlines various lifestyle and environmental factors that can be modified to reduce the risk of sleeplessness. These factors include limiting caffeine after noon, and alcohol use before bedtime, avoiding napping, creating a comfortable sleep environment (preferably no warmer than 65°F), and engaging in regular exercise. While these factors can certainly help promote sleep, they only have a minimal effect when used alone. To achieve the best results, sleep hygiene should be customized to the individual’s specific sleep/wake patterns and paired with other CBT components like SRT or SCT.
Chronic insomnia is one of the most common sleep disorders and a risk factor for several chronic diseases. CBT for insomnia addresses factors that interrupt sleep, making it a better treatment than other short-term treatments like sleeping pills or supplements like melatonin. By understanding the thoughts and behaviors associated with poor sleep patterns, they become easier to identify and replace with habits that promote restful sleep. CBT can benefit anyone who is experiencing sleep problems due to lifestyle habits, medical issues, physical problems, or mental health conditions. It is unique in the sense that it focuses on restricting sleep to promote sleep, it targets stimuli associated with sleep, and it encourages better sleep hygiene practices. CBT is a treatment that should be treated as skill – it requires consistent practice, and while some approaches like SRT may cause initial sleep loss, it can have lasting outcomes not only on sleep quality, but also on overall health.

Monica Echeverri holds a Master of Science in Human Nutrition and Functional Medicine from the University of Western States and currently works as a food photographer, writer, and recipe developer.
✓ This article was reviewed and approved by Emeran Mayer, MD