America’s Falling Life Expectancy

PREMIUM CONTENT for MEMBERS ONLY
We currently live in an amazing period, where medical progress and scientific breakthroughs are celebrated as hallmarks of human advancement. However, to my surprise, even with these amazing advancements, there has been a continuous decline in life expectancy within the United States. Surprisingly, the U.S. now lags behind countries like Cuba, Lebanon, and the Czech Republic in terms of life expectancy. Federal health authorities have reported a second consecutive year of reduced life expectancy, now standing at 76 years, a trend unlike the rebound seen in other countries after the 2020 COVID pandemic. Furthermore, In 2021, maternal mortality rates reached an all-time high, and a publication in the Journal of the American Medical Association (JAMA) disclosed increased mortality rates among U.S. children and adolescents. This has escalated to the extent that American children face a lower likelihood of reaching age 5, compared to those in other high-income nations.
“…Americans continue to experience shorter lifespans and a higher burden of diseases compared to their international peers.”
A decade ago, a group of researchers initiated a study known as “Shorter Lives, Poorer Health” (SLPH). Supported by the National Academy of Sciences and funded by the National Institutes of Health, this study aimed to analyze the disparities in health outcomes between the United States and other developed nations. The findings presented a grim reality, indicating that despite the country’s advancements in science and healthcare expenditure, Americans continue to experience shorter lifespans and a higher burden of diseases compared to their international peers. This is astonishing as the United States has one of the highest costs of healthcare in the world. In 2021, U.S. healthcare spending reached $4.3 trillion, which averages to about $12,900 per person. In 2021, the U.S. spent a whopping 17.8 percent of gross domestic product (GDP) on health care, nearly twice as much as the average OECD country. The OECD (Organization for Economic Co-operation and Development) includes governments of 37 democracies with market-based economies). Health spending per person in the U.S. was nearly two times higher than in the closest country, Germany, and four times higher than in South Korea.
This study underscored the unsettling truth that living in the U.S. poses a health disadvantage and it comes at a very high cost. This disadvantage was found to be evident across all demographics, age groups, and economic strata. It debunked the conventional notion that unhealthy diets and sedentary lifestyles were the sole contributors to poorer health outcomes. Even individuals adhering to healthy behaviors faced elevated disease rates compared to their counterparts in other countries. This disadvantage encompassed a multitude of factors, ranging from individual behaviors, healthcare accessibility, and broader social and environmental determinants of health.
The factors contributing to the declining health in the U.S. are intricate and varied. The “Shorter Lives” report identified several underlying causes:
- Healthcare Access and Disparities: The U.S. “health disadvantage” is characterized by a higher prevalence of chronic diseases and an increased likelihood of premature death. This pattern persists even among those Americans who adopt healthy lifestyles!
- Social Determinants of Health: Elements such as child poverty, racial segregation, social isolation, and the physical environment significantly contribute to health disparities in the U.S. Even urban planning in the country restricts access to nutritious foods, exacerbating the problem (i.e. food deserts, food swamps).
- Injury and Violence: A substantial portion of the life expectancy gap between the U.S. and other nations arises from premature deaths before the age of 50. Factors including drug overdoses, HIV, teenage pregnancies, fatal car accidents, and gun violence all play a significant role.
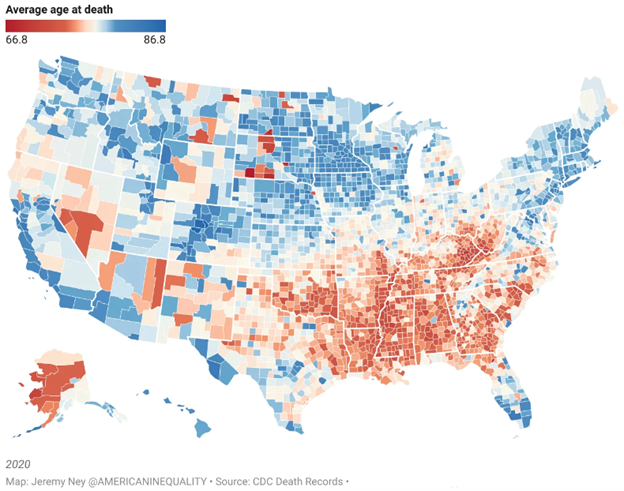
Importantly, these disparities aren’t only between the U.S. and other countries, but also between individual states within the U.S. A recent TIME Magazine article reported that the average age at death had a 20-year gap (see Figure below) and that this divide was largely related to income. In the wealthier areas where median household incomes are in the six figures, Americans live to 87 on average. In poorer areas where median household incomes are on the lower end of five figures, the average life expectancy is 67.
10 years have passed since the release of the SLPH study, yet substantial progress has been limited. The recommended strategies to tackle these issues have seen minimal implementation, leaving the U.S. grappling with a systemic challenge that exceeds even the impact of the recent pandemic. The absence of comprehensive policy responses and reluctance to learn from successful approaches in other countries hinder America’s prospects of reversing this concerning trend.
The decline in life expectancy in the United States signifies more than just a statistic – it mirrors a multifaceted predicament demanding immediate attention. As the United States navigates the complexities of healthcare, societal dynamics, and policy shifts, there is hope that insights from other countries will be embraced, leading to potential solutions that could be implemented here. The well-being of countless Americans hangs in the balance, urging collaborative efforts to regain lost ground and secure a healthier future for those who need it most.

E. Dylan Mayer Dylan is a graduate from the University of Colorado at Boulder, with a major in Neuroscience and minor in Business. He has also recently completed his M.S. in Human Nutrition at Columbia University.
✓ This article was reviewed and approved by Emeran Mayer, MD