A Multidisciplinary Approach to Disorders of Brain-Gut Interaction
PREMIUM CONTENT for MEMBERS ONLY
By Suzanne Smith, MSN, NP, CMT-P
“There is now significant scientific evidence to demonstrate the interactions between the brain, gut and microbiome.”
Have you ever experienced an unpleasant sensation in your gut when you were nervous or frustrated or even thinking about something stressful? That experience is a simple example of how the brain can impact the gastrointestinal system. Even if you do not feel the sensations in your gut, emotions and thoughts have an influence on your gut.
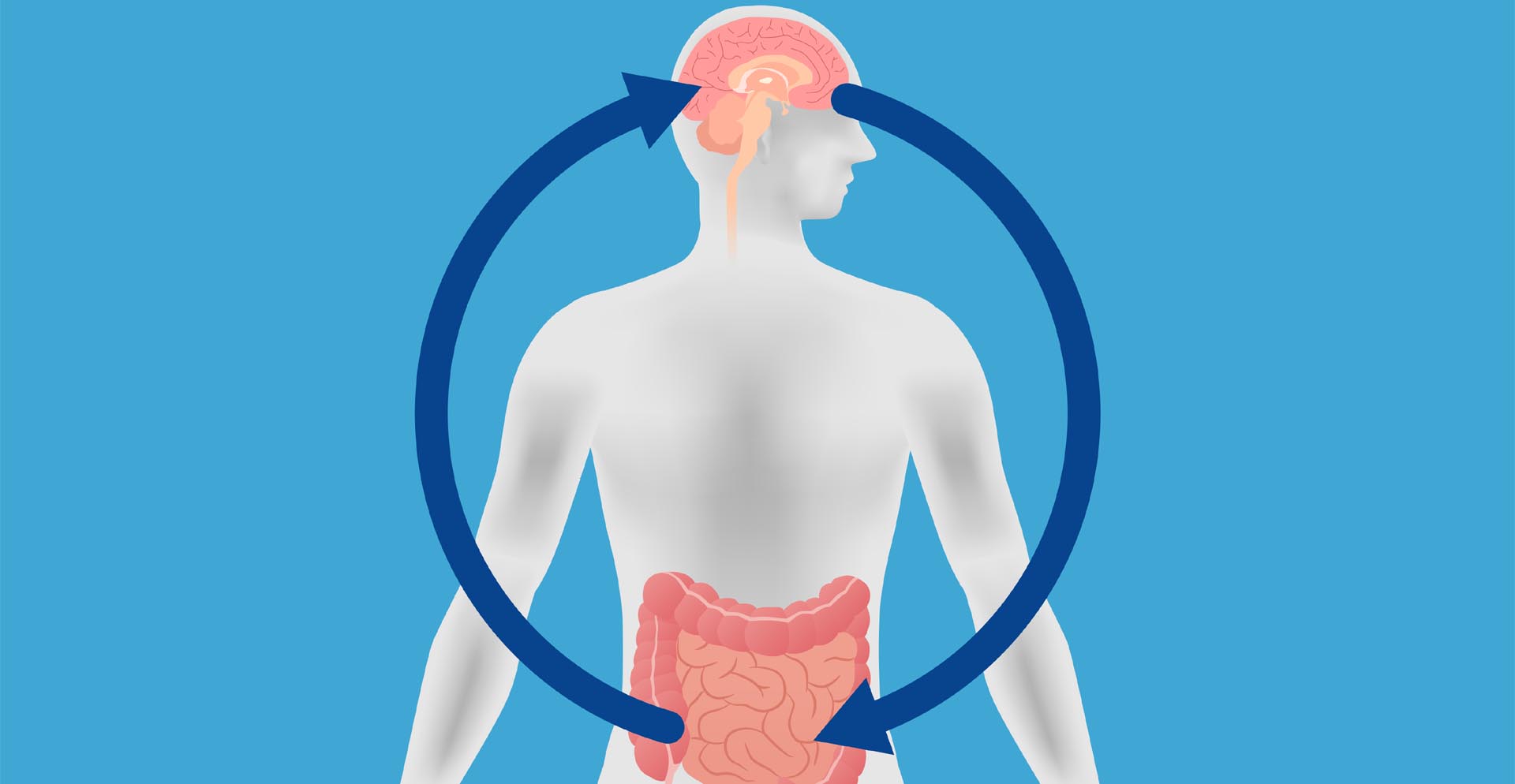
There is now significant scientific evidence to demonstrate the interactions between the brain, gut and microbiome. This intricate communication system that continuously signals back and forth in order to maintain balance is known as the brain-gut-microbiome axis.
Much of the pioneering research on the brain-gut axis was realized under the direction of Emeran Mayer, MD and continues today in collaboration with other investigators at the UCLA G. Oppenheimer Center for Neurobiology of Stress and Resilience.
“When there is a disruption in the brain-gut-microbiome axis … it can express as digestive disorders such as IBS, abdominal bloating, chronic diarrhea and constipation and abdominal pain.”
When there is a disruption in the brain-gut-microbiome axis this can result in alterations in sensory, motor and immune functions expressing as digestive disorders such as IBS, abdominal bloating, chronic diarrhea and constipation and abdominal pain. These disorders often known as Functional Gastrointestinal Disorders were renamed in 2016 to Disorders of Brain-Gut Interaction (DBGI) to reflect the importance of this axis.
When there is irritation in the gut, signals that travel to the brain may alter mood impacting your mental state and in turn this may amplify signals in the gut impacting how you feel physically creating a negative feedback loop that can result in chronic symptoms leading to chronic stress. In addition, lifestyle factors such as sleep, nutrition, stress and exercise play an important role in digestive health. For example, chronic stress impacts the gut microbiome, pain perception and sleep; and conversely sleep impacts the gut microbiome, pain perception and stress.1, 2
When we are stressed or sleep deprived we do not tend to make the healthiest food choices. These lifestyle factors all influence each other and contribute to our state of overall health.
With this evolving understanding of these multiple processes influencing the brain-gut-microbiome axis, it is important to address all factors of digestive health in order to restore or maintain a healthy brain, gut and microbiome.
“At UCLA we have established an Integrative Digestive Health and Wellness program…”
At UCLA in the Melvin and Bren Simon Digestive Diseases Center we have established an Integrative Digestive Health and Wellness program, to approach disorders of brain gut interaction through a biopsychosocial model that offers a personalized and integrative approach, targeting factors that influence the brain, gut and microbiome, thus optimizing overall health.
The program offers a collaborative, team-based approach consisting of gastroenterologists, an integrative health nurse practitioner, registered dietitians, and a GI health psychologist.
The gastroenterologist provides a comprehensive evaluation and manages care. They create a collaborative care plan and refer to the appropriate team members based on contributing factors. They may prescribe medications targeting the brain to help regulate the signaling between the brain and the gut as well as other treatments to improve symptom management.
“The goal is to foster patient empowerment through a personalized care plan based on the patient’s condition, goals and lifestyle.”
As the integrative health nurse practitioner, I provide education about the brain-gut microbiome axis. I offer the patient practical tools and resources for symptom and stress management with a focus on health enhancement such as promoting sleep, exercise, stress management, resilience and self-care. The goal is to foster patient empowerment through a personalized care plan based on the patient’s condition, goals and lifestyle. As a certified mindfulness teacher, I employ mindfulness-based interventions for stress management and relaxation training to better modulate the nervous system. Mindfulness Based Stress Reduction has been shown to decrease symptom severity, improve regulation of attention and emotion and contribute to overall wellbeing in IBS.3, 4, 5
“Nutrition is the foundation for a healthy gut microbiome.”
Nutrition is the foundation for a healthy gut microbiome. Since each person’s microbiome is unique, it is important to personalize nutrition. The certified dietitians in our center have expertise in nutrition for digestive disorders and their nutrition plan focuses on the gut and microbiome. They provide education, guidance and support on dietary modification, regulating bowel habits and symptom management that is supported by research and tailored to each person’s condition and lifestyle.
“…a large body of evidence to support the effectiveness of psychological treatments for digestive disorders…”
There is a large body of evidence to support the effectiveness of psychological treatments for digestive disorders especially disorders of brain-gut interaction. The GI Health psychologist is specially trained in these gut-directed evidence-based psychological treatments to influence the brain-gut connection such as Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy and medical hypnosis. The GI health psychologist develops a plan based on the needs of the patient that not only addresses symptoms but also promotes meaningful living while learning to manage their condition.
Recently in 2020, a study of an open-label, single-center, randomized controlled trial comparing standard care to multidisciplinary care for disorders of brain-gut interaction in a gastroenterology clinic was published. The authors found that 84% of patients treated with a multidisciplinary care team reported global symptom improvement compared to 57% of patients treated with standard care. Those in the multidisciplinary group also reported greater improvement in psychological well-being, with a 40% decrease in depression, compared with a 9% decrease for those in standard care.6
If you are living with a digestive disorder that impacts your quality of life and you find stress, diet and other factors exacerbate your symptoms, you may be a candidate for our program.
Please visit our Integrative health and wellness program website:
https://www.uclahealth.org/gastro/gi-wellness
if you would like to partner with our multidisciplinary team in managing your disorder, make an appointment with one of our gastroenterologists for an evaluation and to inquire about a referral.
https://www.uclahealth.org/gastro/ibs
Wishing you wellness.
References
- Wang Y et al, Brain Behav Immun. 2014
- Li Y et al, Front Psychiatry. 2018
- Zernicke et al, J Behav Med. 2013
- Gaylord et al, Am J Gastroenterol 2011
- Naliboff et al, Neurogastroenterology & Motility, 2020
- Basnayake et al, J Gastroenterol Hepatol. 2020
 Suzanne Smith, MSN, NP, CMT-P is nurse practitioner at UCLA where she heads the Integrative Digestive Health and Wellness Program, teaching mind-body based skills and promoting healthy living for gastrointestinal conditions. She is a regular contributor to the MGC Blog.
Suzanne Smith, MSN, NP, CMT-P is nurse practitioner at UCLA where she heads the Integrative Digestive Health and Wellness Program, teaching mind-body based skills and promoting healthy living for gastrointestinal conditions. She is a regular contributor to the MGC Blog.